CUSTOMER CHALLENGE
Located at Orthopaedic Hospital in affiliation with the Department of Orthopaedic Surgery at the University of California Los Angeles (UCLA), the Implant Performance Lab provides research and education in the field of orthopaedic implant biomechanics. The group specializes in understanding and simulating the in-vivo performance of orthopaedic implants, by identifying the key relationships between implant biomechanics, surgical techniques and clinical outcome, and by building models to study these interactions. The team subjects devices to the forces and moments that they will experience during clinical use, with the goal of accurately predicting clinical performance.
Implant developers run a large variety of strength, fatigue and wear tests to understand and characterize the predicted device performance. These results often become part of the body of information that is submitted during the regulatory approval process.
“These tests are essential for getting a device to the marketplace, but this type of testing needs to be constantly updated and improved to ensure that the device will be free of other problems over time,” said Sophia Sangiorgio, PhD, Implant Performance Lab. “For example, with a total hip replacement, fatigue failure of the femoral stem was somewhat common in the 1970s. As a result, femoral stems today are manufactured to have excellent resistance to fatigue fracture.
“However, over the years, patients’ expectations and activity levels have increased, leading to other types of implant failure, such as loosening or dislocation, which is equally as catastrophic for the patient as a stem breaking,” Sangiorgio added. “We are focused on scenarios like this to help surgeons and device developers improve outcomes for patients.”
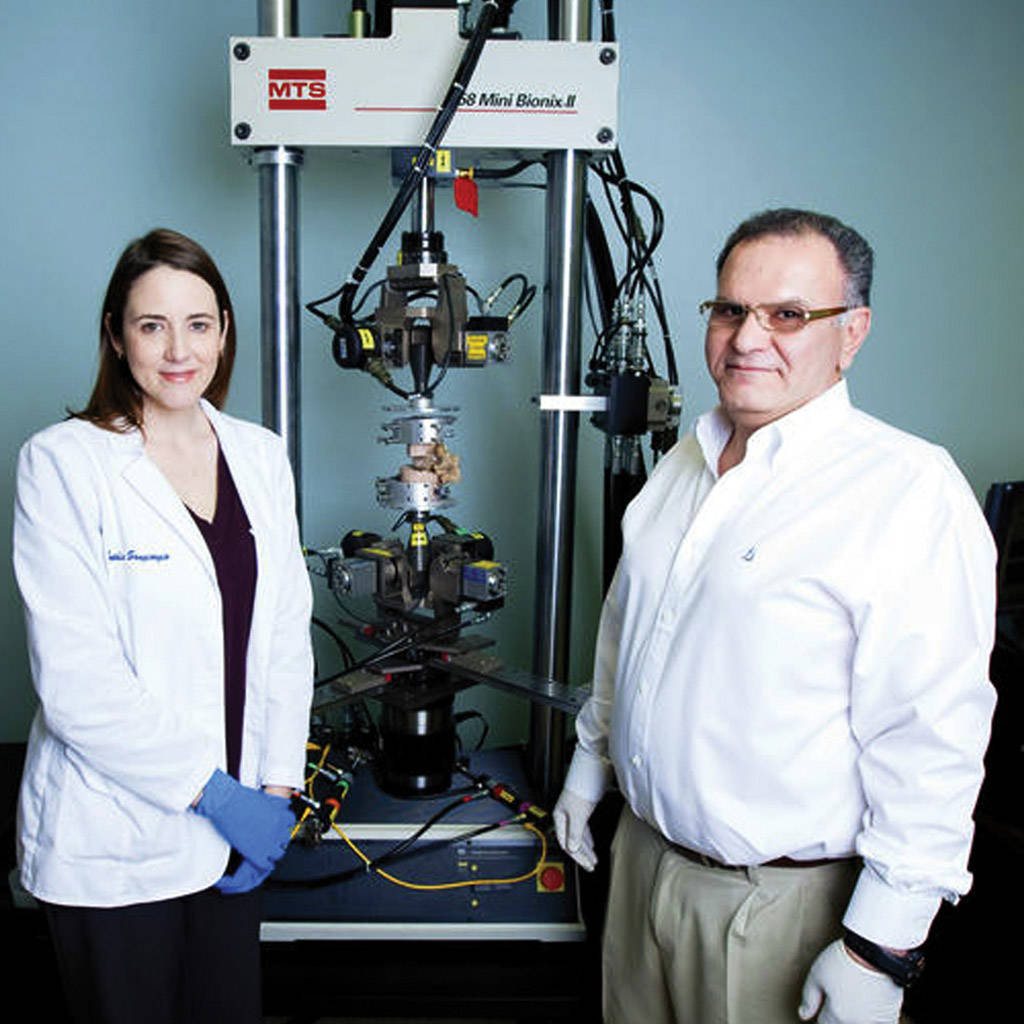
The Implant Performance Lab is one component of the J. Vernon Luck Orthopaedic Research Center at Orthopaedic Hospital, which comprises a number of labs specializing in different aspects of orthopaedic research. These include bearing surface tribology, wear particle analysis, implant retrieval analysis, biomechanics of healing of bone and connective tissues, and computer modeling. According to Eddie Ebramzadeh, PhD, Director of the Implant Performance Lab, mechanical testing offers several advantages over other approaches in assessing implant performance.
“Animals are too small, evaluating prototypes in patients is not appropriate, and it is often difficult to use computer-based models to replicate the highly complex biological environments involved with the human musculoskeletal system,” Ebramzadeh said. “But mechanical modeling is ideal for our work, because in the body, bone, muscle and tissue interact in a mechanical manner. However, the success of this approach depends upon how accurately and reproducibly we can design and conduct our mechanical tests.”
MTS SOLUTION
The Implant Performance Lab employs a variety of MTS load frames, test software and control systems to support its biomechanical testing. Orthopaedic devices under development are implanted in either synthetic bones or cadaveric constructs, which are then mounted in the test systems with custom-designed fixtures and subjected to physiological loads and motions, sometimes over thousands or even millions of cycles.
The team’s research touches practically all areas of the human musculoskeletal system, including the hip, knee and ankle joints, as well as the spine, femur, tibia, elbow and hand.
Five mechanical test stations currently support a busy experimentation schedule, including two uniaxial load frames, one of which has been converted to a custom disc arthoplasty wear simulator, along with a fretting wear simulator for modeling micromotion at implant fixation interfaces. A biaxial load frame is also used for evaluating the fixation and stability of arthroplasties for the hip, knee and spine. The biaxial system is used to apply torsion and axial loads, and the custom rigs allow application of bending moments and other complex physiological load protocols specific to each anatomic location.
The lab is also equipped with a six-station MTS Spine Disc Wear Simulator and an MTS Spine Kinematics Test System, which facilitates simulations in a full eight degrees of freedom. These systems are used to evaluate different designs of posterior dynamic stabilization devices for the lumbar spine. Recently, the researchers have been evaluating different surgical techniques for correcting spine deformity in adolescents, a complex biomechanical problem.
“Our mechanical test equipment gives us confidence in our ability to accurately and reproducibly simulate in-vivo and surgical conditions for many joint replacement implants and fracture fixation devices,” Sangiorgio said.
CUSTOMER BENEFITS
According to Ebramzadeh, his team’s current mechanical testing capabilities align well with the laboratory’s emphasis on resolving day-to-day issues that are of immediate interest to the orthopaedic community.
“We are well equipped to support our emphasis on practical clinical application,” Ebramzadeh said. “Our capabilities allow us to evaluate implant device performance in a manner that will best serve orthopaedic surgeons and their patients.
“Combined with the experienced team of engineers, biologists and surgeons who are active in the Luck Research Center, we are able to provide research that is valuable to the orthopaedic community,” Ebramzadeh continued. “We have earned a reputation for delivering test data that are highly predictive of how an implant will perform over its functional life.”
The Implant Performance Lab has also become a coveted place for Los Angeles-area engineering students to intern. Sangiorgio attributes this appeal to the translational nature of the work.
“Students have the opportunity to work with the latest orthopaedic technology and obtain realistic, hands-on experience that is not available in engineering programs that primarily focus on theory,” Sangiorgio said. “It is readily apparent how our research can improve a patient’s quality of life, and that makes the work both exciting and meaningful for everyone involved.”

